Radiotherapy
Experimental Medical Physics
We pioneer innovative radiotherapy technologies such as FLASH and microbeam therapy to improve cancer treatment — bridging experimental physics and clinical application."
X-ray microbeam radiation therapy (MBT) has been recognised as a unique therapeutic opportunity to alleviate the fundamental dose limitation. In MBT the treatment dose is modulated on the micrometre scale into planar, high dose “peaks” of a few micrometres width separated by a few 100 µm wide low dose regions called “valleys”. Preclinical studies have clearly demonstrated that MBT, with its spatial dose fractionation at the micrometre range, induces pronounced cytotoxic effects on tumour tissue while healthy tissues show a remarkably high functional tolerance, even after irradiation with MBT peak doses of up to 5000 Gy and associated dose rates of several kGy.s-1. Differences in the microenvironment of tumour and normal tissue, such as the immune system, the vasculature and intercellular signalling cause this differential effect.
FLASH radiation therapy is another innovative treatment strategy that uses dose rates above 100 Gy/s compared to conventional radiation therapy with dose rates in the order of a few Gy/min. FLASH irradiation showed in preclinical and recently first clinical applications strongly reduced adverse effects on normal tissue at equal doses, while the effect on the tumour remained unimpaired. The astonishing results of the first experiments with FLASH radiation therapy rapidly triggered a strong medical and commercial interest.
FLASH and MBT are two exciting new developments in radiation oncology that have not yet reached clinical standard. A lack of mechanistic understanding for their effectiveness, challenges in dosimetry and quality assurance, and most importantly the unavailability of radiation sources facilitating the treatments are preventing the clinical translation.

Until recently, x-ray microbeam radiation therapy and x-ray FLASH therapy have only been possible at large synchrotrons, which are huge research facilities. We developed in our team compact alternatives and hence enable preclinical research independent of synchrotrons. We want to go further:
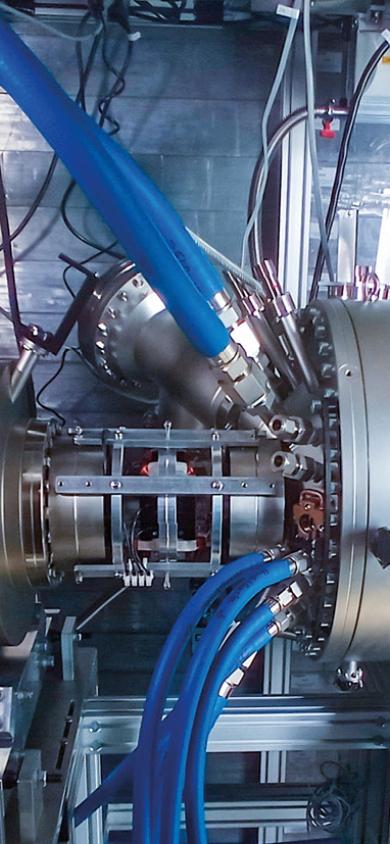
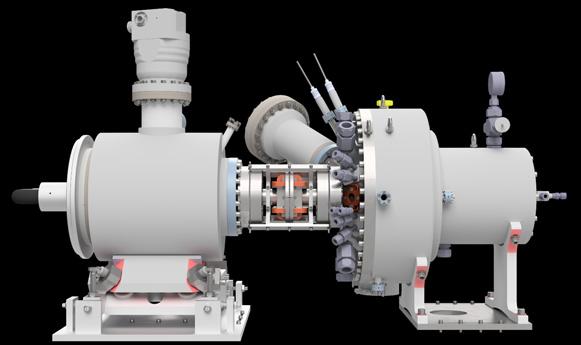
One of my primary objectives for the next five years is the set-up of the first clinically applicable microbeam radiation source based on line-focus X-ray tube technology. This technology enables x-ray beams from micrometre sized emitters (i.e. spatially coherent x-rays) with doses of several 10 probably up to 150 Gy/s.
This ambitious deep-tech project brakes current x-ray tube records by orders of magnitude and involves innovative tools in electron acceleration and focusing in collaboration with the University of Mainz, enhancing the structure and material combinations in the X-ray target in partnership with the Research Centre Jülich, and establishing a modular pulsed high-voltage source in cooperation with the Hochschule München.
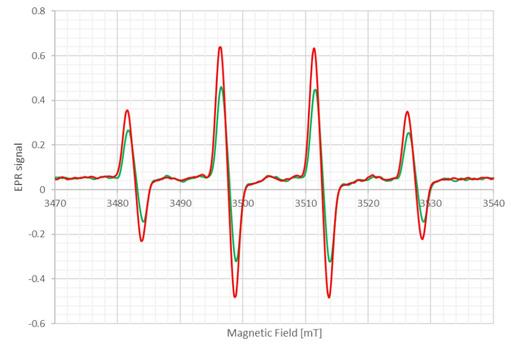
Understanding the underlying mechanisms of FLASH therapy and spatially fractionated radiation therapy is crucial to optimizing treatment efficacy. To this end, we are investigating the role of radiochemical interactions involving reactive oxygen species (ROS), examining the influence of radiochemical levels in cells and tissues on biological response, and analysing the impact of high-dose rates, radiation doses, and spatial fractionation on cell metabolism and intercellular signalling such as bystander effects. We employ various assays to detect ROS experimentally, for example by employing spin traps and electron spin resonance measurements.
Radiochemistry plays a major role between a few nanoseconds up to around 1 second after radiation absorption. There is growing evidence that this phase is crucial for an understanding of radiation therapy at high dose rates and spatial fractionation. Apart from experimental measurements of radiochemical species, we develop models of the evolution of reactive radiochemical species.
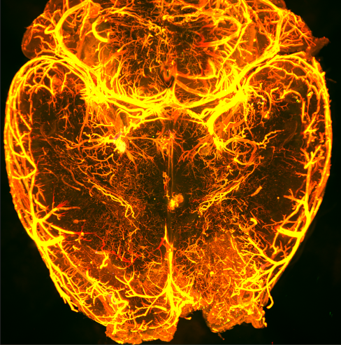
The success of radiation treatment depends strongly on the tissue and tumour microenvironment – intracellular signalling, immune system, vasculature and oxidative stress. We aim to understand novel treatment strategies, such as FLASH and microbeams better by performing preclinical in vitro and in vivo studies. With various cutting-edge imaging techniques we decipher the secrets of radiation action in cells and tissue.
Focus of our investigations are radio-immune interactions in microbeam and minibeam radiation therapy, bystander signalling and oxidative stress and the role of vascular damage for the efficacy of microbeam radiation therapy.
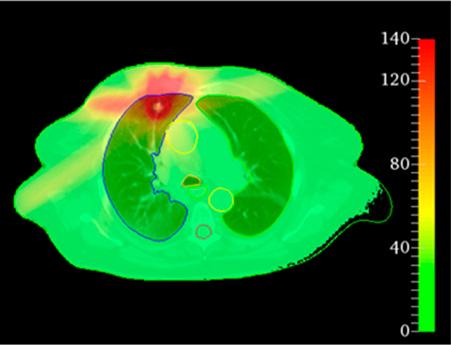
Treatment planning is an essential step before any state-of-the-art radiotherapy treatment: It is required to estimate tumour control and potential side effects in organs at risk. In our team we develop innovative methods for dose calculation and biologically motivated treatment planning in spatially fractionated radiation therapy.
Part of the teams work is the implementation of fast and accurate dose calculation methods and a detailed characterization of source parameters. Together with partners at the Australian Synchrotron, we embedded these tools in a professional treatment planning system and we are now adapting it to our compact microbeam sources. The developed tools are used for retrospective treatment planning studies with the aim to establish the relevant field parameters and identify patient cohorts for first clinical applications in microbeam radiation therapy.
Dosimetry and quality assurance with micrometre sized beams is challenging. We established film dosimetry protocols with microscopic read-out and test various high-resolving dosimeters for future clinically relevant quality assurance protocols.
| Postdocs: | PhD students: | Master students: |
|
|
|
Our team is located at the Department of Radiation Oncology at the University Hospital rechts der Isar of the Technical University Munich (TUM) and the Institute of Radiation Medicine at the Helmholtz Centre Munich, lead by Prof. Dr. Stephanie Combs.
We are situated at three different sites in Munich:
Ismaninger Straße 22
81675 Munich
Building UYM
Lichtenbergstraße 1
85748 Garching
Institute for Radiation Medicine
Ingolstädter Landstraße 1
85764 Oberschleißheim
Telephone:
E-Mail: